
Surgical Solutions: Exploring Hysterectomy As A PCOS Treatment
Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read MoreThe question of can you get pregnant with endometriosis touches the lives of many women. Endometriosis, a condition comprising tissue comparable to the interior lining of the uterus grows outside of it, often leads to fears about fertility. While it can present hurdles on the path to pregnancy, many women with endometriosis do successfully conceive, although they may navigate a more challenging journey to parenthood.
At The Women’s Center, we understand the complexities of trying to conceive with a diagnosis of endometriosis. That’s why our endometriosis specialist in Orlando approaches your care with empathy and expertise. We tailor our fertility treatments to work with your body’s unique situation, employing cutting-edge medical interventions and personalized support, to enhance your chances of a successful pregnancy.
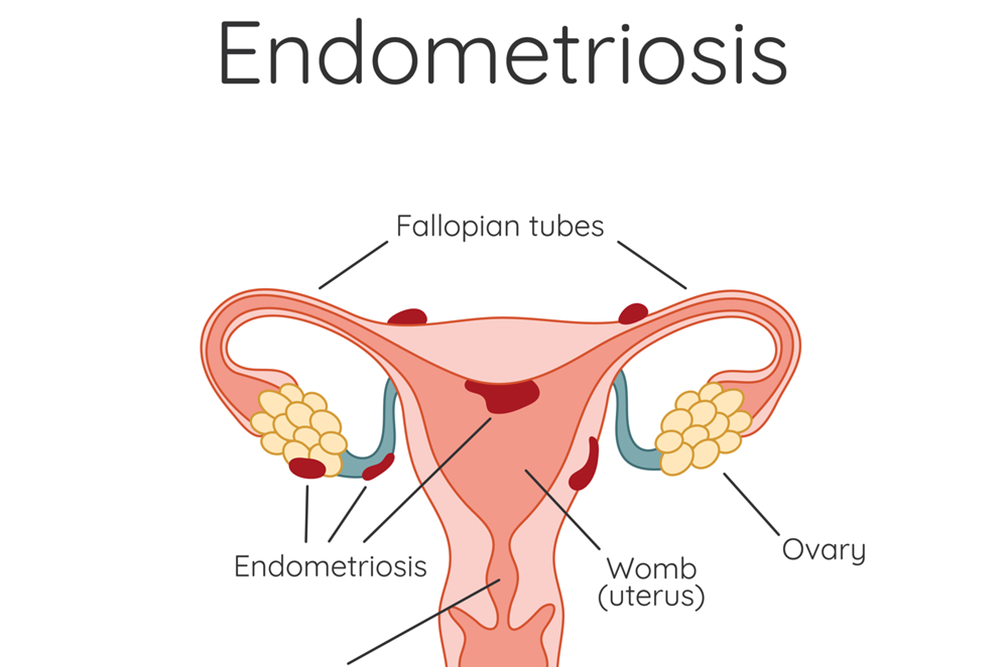
The conundrum of conceiving with endometriosis is as complex as the condition itself, arrayed with a multitude of factors that play into fertility. Many women carrying the weight of this diagnosis find solace in the fact that their dream of motherhood may still be within reach. Fertility may be hampered, as endometrial tissue can disrupt the meticulous orchestration of the reproductive system, causing inflammation and scarring that might impede the journey of the egg or sperm.
Nonetheless, conception remains a tangible prospect for those with mild to moderate manifestations of the condition. With comprehensive support from dedicated healthcare providers, women can explore various avenues to alleviate the symptoms that may be hindering conception, guiding them closer to achieving pregnancy.
The pursuit of pregnancy for women with endometriosis often begins with an open and honest consultation with a healthcare provider well-versed in the condition's nuances, ready to offer a medley of interventions ranging from medication to lifestyle adjustments. These professionals serve as navigators through the choppy waters of reproductive challenges, charting a course that enhances the likelihood of conception. By crafting individualized care plans and monitoring progress meticulously, women can find solace in the knowledge that their health and their aspirations are being honored and addressed with utmost care.
The narrative of endometriosis and fertility is not solely one of despair; it is punctuated with stories of tenacity and success. The condition may cast a shadow on fertility rates, with some forced to grapple with the harsher realities of blocked fallopian tubes or compromised ovarian function, yet a complete impediment to pregnancy it is not.
For every fallopian passage obstructed, there lies a spectrum of fertility potential that varies as widely as the symptoms of the condition itself. Fostering an understanding of one's body through methods such as fertility tracking and hormonal assessments, women can unearth insights into their personal fertility landscape, illuminating paths to pregnancy that may have otherwise remained in the dark.
A comprehensive approach to managing one's reproductive health is pivotal in mitigating the impact of endometriosis on fertility, encompassing both medical attention and resolute personal determination. Women are often surprised to find that surgical interventions, while daunting, have the potential to clear the way for pregnancy, removing barriers posed by the errant tissue. A diligent follow-up with healthcare specialists can ensure that recovery is on track and fertility potential is maximized, providing a robust foundation for attempting conception.
For many women facing the trials of endometriosis, it is the advent of fertility treatments that heralds a new chapter in their reproductive story. Assisted reproductive technologies, such as in vitro fertilization, offer a ray of hope, unlocking doors to motherhood that seemed insurmountable.
IVF circumvents the anatomical impediments of endometriosis, creating an environment in which the egg and sperm can unite unencumbered by the ailment's complications. Prior to embarking on fertility treatments, the surgical removal of problematic endometrial tissue can improve the odds, setting the stage for a more successful conception attempt.
Engaging with a fertility specialist, one seasoned in the subtleties of reproductive care, is a critical step in enhancing pregnancy outcomes for those with endometriosis. Such experts not only bring a wealth of knowledge but also a compassionate understanding of the emotional rollercoaster many patients experience. They are prepared to tailor treatment regimes, combining the latest advancements in medical science with a personal touch, aiming for the best possible result—a successful pregnancy.
As women tread the path to parenthood, these specialized treatments serve as beacons of hope, signifying that even amidst the challenges of endometriosis, the dream of pregnancy is far from unattainable.
Our commitment to supporting women doesn’t end at diagnosis. The Women’s Center is dedicated to helping you overcome the challenges of endometriosis and move closer to fulfilling your dream of becoming a parent. Through a combination of advanced reproductive technologies and holistic care frameworks, we strive to provide not just treatments, but hope and empowerment for every woman walking through our doors.
At The Women’s Center, we prioritize your overall well-being, offering comprehensive services including obstetrics, gynecology, and medical aesthetics. Since 2001, we’ve stood by the women of Central Florida as their trusted family health partner, with our doors open across 9 convenient locations.



Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read More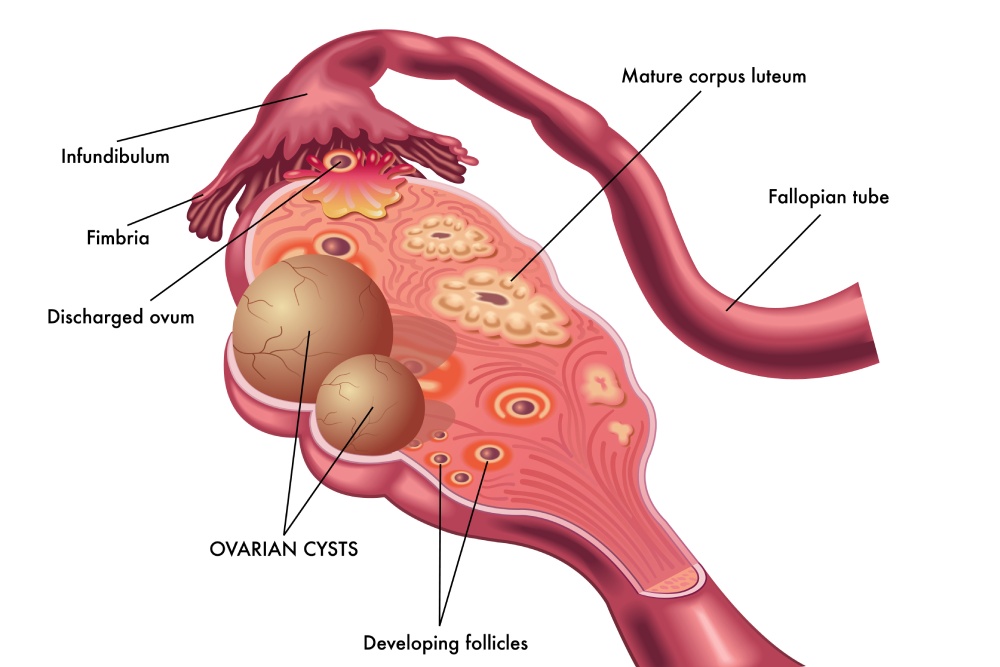
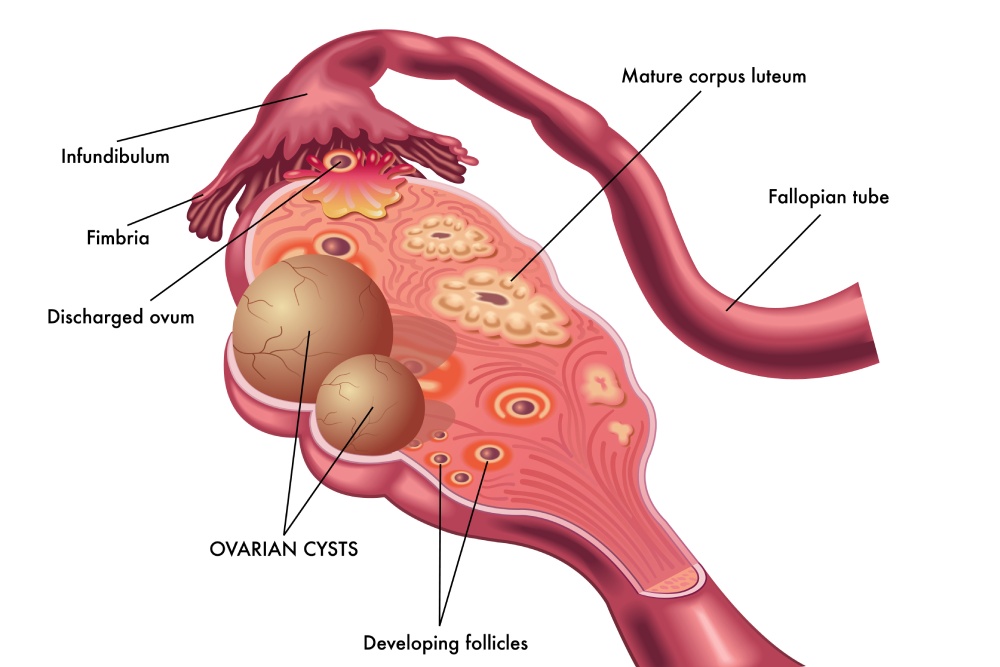
Ovarian cysts after menopause may seem uncommon, but they can still develop even when the...
Read More
Uterine fibroids are one of the most common benign growths affecting women. By age 50,...
Read More