
Surgical Solutions: Exploring Hysterectomy As A PCOS Treatment
Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read MorePolycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal imbalance, and fertility struggles. When symptoms grow severe or resistant to treatment, some women begin exploring surgical options. For some women, hysterectomy is considered as a potential option for long-term symptom relief.
However, a hysterectomy for PCOS is a complex decision that extends beyond symptom control. Understanding the pros and cons of hysterectomy for PCOS is important before moving forward with such a life-changing choice.

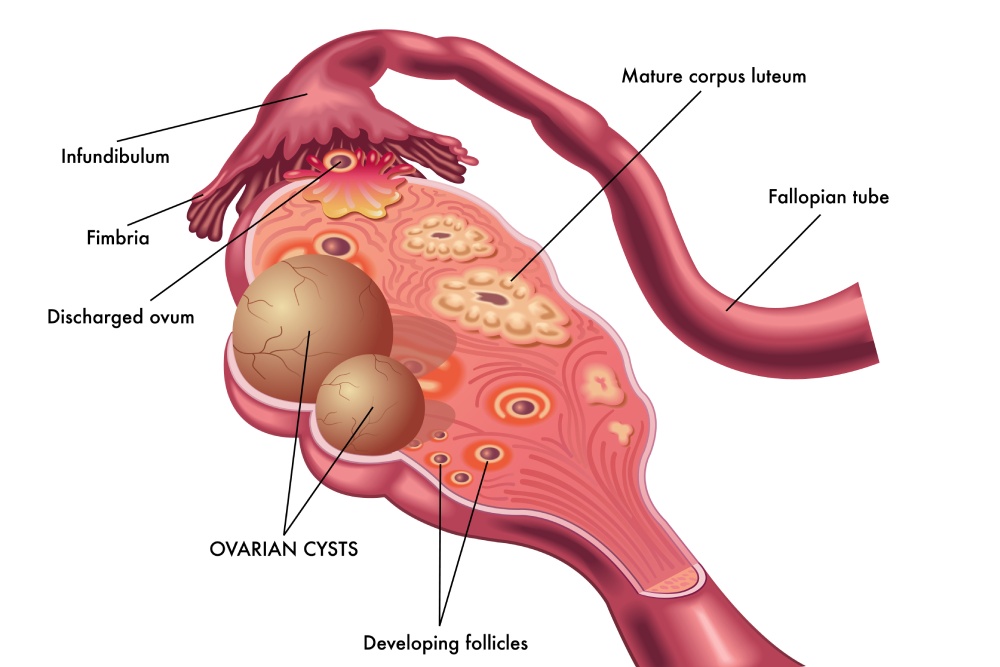
Polycystic Ovary Syndrome (PCOS) is a hormonal condition that affects how the ovaries function. It disrupts normal ovulation, leading to irregular or missed menstrual cycles. Many women also experience excess hair growth, acne, and weight gain caused by higher androgen levels.
Beyond reproductive symptoms, PCOS can affect overall health. It increases the risk of insulin resistance, diabetes, and high cholesterol. Over time, prolonged hormone imbalance may cause the uterine lining to thicken, raising concerns about endometrial hyperplasia or cancer.
PCOS is challenging because it originates from hormonal imbalances, not the uterus itself. It begins with the hormonal interaction between the ovaries, adrenal glands, and brain. This distinction is vital when discussing hysterectomy. Removing the uterus may address certain complications like heavy bleeding, but it does not correct the underlying hormone imbalance driving PCOS.
That is why most women work closely with a PCOS Specialist to manage their symptoms through medication, hormone therapy, and lifestyle changes before exploring surgery. The goal is to control hormonal triggers and protect reproductive and metabolic health for the long term.
A hysterectomy is a surgical procedure that removes the uterus. Depending on the individual’s condition, it may also involve removing other reproductive organs. The type of hysterectomy performed depends on the symptoms, diagnosis, and desired outcome.
In a total hysterectomy, both the uterus and cervix are removed. A partial or subtotal hysterectomy removes only the uterus, leaving the cervix intact. In some cases, surgeons may perform a total hysterectomy with bilateral salpingo-oophorectomy, which removes the uterus, fallopian tubes, and ovaries.
Hysterectomy is often recommended for conditions such as fibroids, severe bleeding, endometriosis, or uterine cancer. For women with PCOS, it may be considered if the condition causes ongoing endometrial thickening, chronic pain, or bleeding that does not respond to medication.
It is important to recognize that a hysterectomy is not a primary treatment for PCOS. Since PCOS develops from hormonal imbalance, surgery targets only uterine complications and not the root hormonal causes. However, for some women, it can bring meaningful relief when combined with hormone management and regular follow-up care.
To better understand surgical options and recovery expectations, consulting a Hysterectomy Specialist helps clarify which approach may fit your individual needs and health goals.
A hysterectomy is rarely the first step in managing PCOS. It is generally considered after other treatments have failed or when complications place a woman’s health at risk.
One common reason is persistent heavy bleeding. Chronic anovulation causes the uterine lining to build up without regular shedding, leading to prolonged or painful periods. If hormone therapy and medication do not control the bleeding, hysterectomy may be discussed as a final option.
Another reason involves endometrial hyperplasia, a thickening of the uterine lining caused by excess estrogen. In some women, this condition can increase the risk of developing endometrial cancer. Removing the uterus eliminates that risk and may offer peace of mind.
A hysterectomy for PCOS may also be considered when other uterine conditions such as fibroids or adenomyosis cause significant discomfort. For women nearing menopause, the procedure may help reduce pain and heavy bleeding while also lowering cancer-related risks.
Still, this decision requires careful evaluation. The uterus plays no direct role in hormone production, so surgery does not treat the hormonal aspects of PCOS. And if the ovaries are left intact, symptoms like acne, hair growth, and insulin resistance may continue.
Because of these complexities, doctors often recommend thorough testing before surgery. Imaging studies, biopsies, and hormone assessments can help determine if hysterectomy is truly appropriate. A thoughtful conversation with your gynecologist can help weigh all options and consider how the procedure fits your long-term health plan.
A hysterectomy for PCOS may be performed in several ways depending on your health, anatomy, and the extent of removal needed. Understanding what happens during the procedure can help you prepare both physically and emotionally.
In a laparoscopic hysterectomy, small incisions are made in the abdomen to insert surgical instruments and a camera. This minimally invasive method usually results in less pain, smaller scars, and quicker recovery. A vaginal hysterectomy removes the uterus through the vagina and does not require abdominal cuts, making it another less invasive option for qualified patients.
For complex cases or when larger organs must be removed, an abdominal hysterectomy may be required. This involves a larger incision across the lower abdomen and typically demands longer healing time.
During surgery, anesthesia is used to keep you asleep and comfortable. Depending on your condition, your surgeon may remove just the uterus or include the cervix, ovaries, and fallopian tubes. The operation usually lasts between one to three hours.
After surgery, most women stay in the hospital for one to two days. Pain, fatigue, or mild bleeding may occur, but these symptoms gradually improve with rest. Full recovery can take several weeks depending on the surgical method used.
Deciding on a PCOS hysterectomy is deeply personal and depends on your medical history, age, and long-term goals. It offers both advantages and disadvantages that must be weighed carefully.
For some women, hysterectomy brings freedom from years of heavy bleeding, pelvic pain, or uterine discomfort. By removing the uterus, the risk of endometrial cancer drops significantly, which can be reassuring for those with long-standing hormonal imbalance. When the ovaries are also removed, symptoms linked to estrogen dominance, such as endometrial thickening or chronic bleeding, may improve.
Another benefit is the elimination of menstrual bleeding, which many women with PCOS find unpredictable or painful. For women who no longer plan to conceive, this outcome can simplify their lives and bring emotional relief from the stress of irregular cycles. Some also report reduced pelvic discomfort and improved quality of life after recovery.
Despite these improvements, hysterectomy is not a cure for PCOS. The condition involves hormone production, and removing the uterus does not correct that imbalance. If the ovaries are preserved, androgen-related symptoms such as acne, excess hair growth, and weight fluctuations may continue.
If both ovaries are removed, surgical menopause occurs immediately. This sudden drop in estrogen can cause hot flashes, mood swings, vaginal dryness, and increased risk of osteoporosis. Hormone replacement therapy may help ease these effects but must be managed under medical supervision.
Additionally, every surgery carries risks of infection, bleeding, or reactions to anesthesia. Physical and emotional recovery may take longer than expected. For this reason, hysterectomy is generally viewed as a last resort, not a first-line treatment for PCOS.
Recovery after a hysterectomy for PCOS varies depending on the type of surgery and how your body responds. Most women experience physical healing within six to eight weeks, but internal recovery and hormonal adjustments can take longer.
Immediately after surgery, you may feel tired and sore. Light walking can help prevent blood clots and support circulation, but rest remains important. Heavy lifting or intense activity should be avoided until your doctor confirms full healing. You may also notice changes in your mood, appetite, or sleep patterns as your body adjusts.
If your ovaries are removed during surgery, menopause begins instantly. This is known as surgical menopause, and it often brings stronger symptoms than natural menopause. Hot flashes, vaginal dryness, or mood changes can appear suddenly. Because estrogen levels drop sharply, your doctor may discuss hormone replacement therapy (HRT) to manage these symptoms and support bone health.
For women who keep their ovaries, hormonal shifts occur more gradually. You may still ovulate irregularly for a while, though menstruation stops since the uterus is gone. However, PCOS-related symptoms like acne, hair thinning, or weight fluctuations may persist due to ongoing androgen production from the ovaries and adrenal glands.
A common question is whether a hysterectomy can cure PCOS. The simple answer is no. PCOS is an endocrine disorder, not a uterine one. The hormonal imbalance originates from how the body produces and regulates insulin, androgens, and other reproductive hormones, not from the uterus itself.
Because of this, removing the uterus does not stop the overproduction of androgens or insulin resistance. Women who undergo hysterectomy may still face metabolic challenges such as high blood pressure, elevated cholesterol, or prediabetes. These conditions are tied to how the body processes sugar and fat, not to the uterus or menstrual cycle.
Even after surgery, symptoms like unwanted hair growth, acne, or weight changes may continue if the hormonal imbalance remains untreated. The adrenal glands, for example, still release testosterone and other androgens that contribute to these effects.
What a hysterectomy can do, however, is relieve symptoms linked to uterine complications such as prolonged bleeding, pain, or risk of endometrial cancer. It can also make symptom management easier for women approaching menopause or facing multiple gynecologic conditions.
To manage the full spectrum of PCOS, women often need a comprehensive plan that includes nutrition, exercise, medication, and hormonal care.
While hysterectomy is not a cure for PCOS, it can be the right choice for women whose quality of life is deeply affected by severe uterine or hormonal complications. Doctors typically recommend it only after exploring every other possible treatment.
A hysterectomy may be considered if you experience uncontrollable bleeding, chronic pelvic pain, or have developed conditions such as endometrial hyperplasia, fibroids, or uterine prolapse. These problems often worsen PCOS symptoms and can become dangerous if left untreated. Removing the uterus can stop persistent bleeding and relieve pelvic pressure, giving you lasting physical comfort.
For some women, the decision also depends on age and fertility goals. If you have completed your family or are approaching menopause, a hysterectomy may help you move forward without the monthly discomfort or anxiety tied to abnormal cycles. When combined with removal of the ovaries, it can also reduce the risk of certain ovarian cancers. However, this step causes immediate menopause and requires thoughtful discussion about hormone therapy.
Emotional readiness is equally important. Undergoing a hysterectomy changes your body and fertility, so counseling or support groups can help you process these feelings and make a confident decision.
Ultimately, the right approach is highly personal. Your healthcare provider will assess your medical history, test results, and long-term goals before deciding if surgery fits your needs. In cases where symptoms are manageable with lifestyle and medication, less invasive treatments remain the preferred route.
For many women, a hysterectomy for PCOS may feel like a last resort. In reality, several effective alternatives can help manage symptoms, regulate hormones, and improve quality of life without surgery.
The first line of treatment often includes lifestyle modifications. Maintaining a balanced diet, increasing physical activity, and managing weight can significantly reduce insulin resistance and improve ovulatory function. These changes help stabilize hormone levels, which may reduce irregular bleeding and pain.
Hormonal therapy is another common treatment option. Birth control pills, progestin-releasing IUDs, or hormone patches can help regulate menstrual cycles, reduce uterine lining buildup, and prevent heavy bleeding. These methods are usually considered before surgery, as they address hormonal imbalance, which is the main cause of most PCOS-related complications.
For women with fertility concerns, ovulation-inducing medications such as letrozole or clomiphene citrate may help restore regular cycles and increase the chance of conception. In some cases, doctors may recommend metformin, a medication that improves insulin sensitivity and supports hormonal balance.
Here at The Women’s Center, we understand that living with PCOS can be overwhelming, especially when symptoms begin to affect your daily life and overall well-being. Our compassionate team helps you explore every option, from lifestyle guidance to advanced surgical solutions, so you can make informed decisions about your health.
With specialized care across Central Florida, we are here to help you regain balance and confidence through personalized women’s health care.



Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read More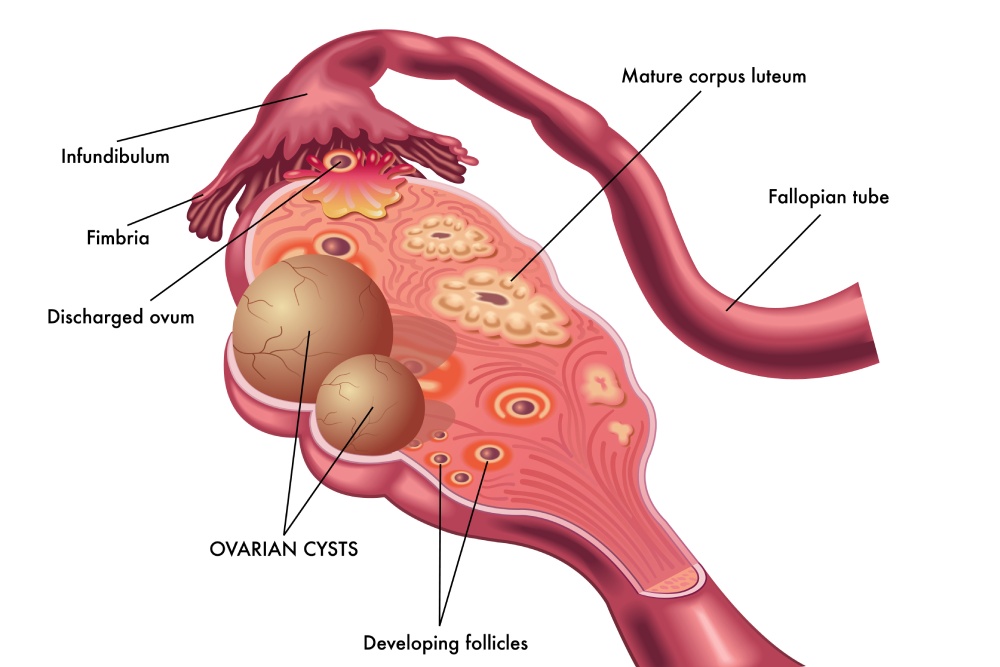
Ovarian cysts after menopause may seem uncommon, but they can still develop even when the...
Read More
Uterine fibroids are one of the most common benign growths affecting women. By age 50,...
Read More