
Surgical Solutions: Exploring Hysterectomy As A PCOS Treatment
Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read MoreOvarian cysts after menopause may seem uncommon, but they can still develop even when the ovaries are less active. Many women may wonder if ovarian cysts can still develop after menopause. The answer is yes, though the types of ovarian cysts after menopause and their risks differ from those in younger women.
Knowing these changes helps you spot symptoms early and take timely action for your health.
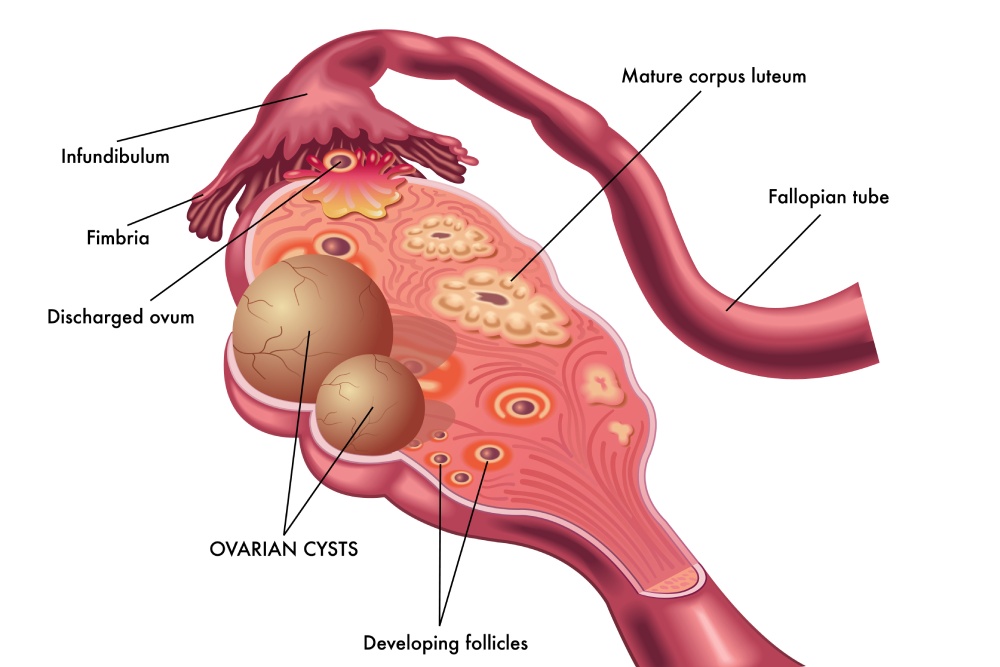
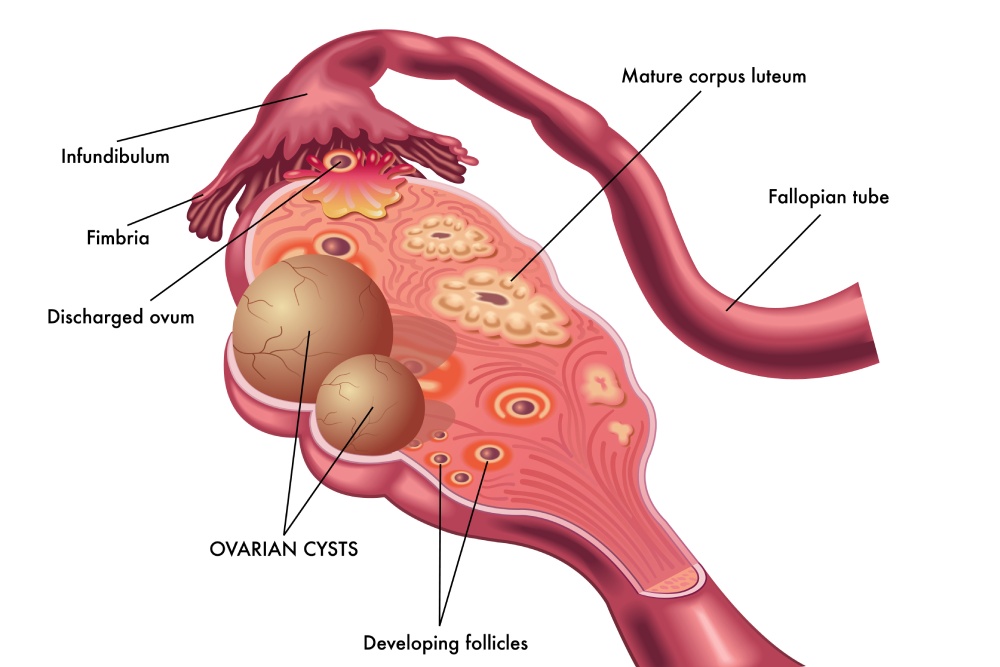
An ovarian cyst is a fluid-filled sac that forms in or on the ovary. Before menopause, these cysts are often linked to the menstrual cycle, appearing as part of normal ovulation. After menopause, the ovaries stop releasing eggs and hormone production slows, yet cysts can still form.
Common postmenopausal cyst types include dermoid cysts, which develop from cells present since birth, and cystadenomas, which grow on the surface of the ovary. Although most cysts are noncancerous, the chance of malignancy increases slightly with age.
Research indicates that postmenopausal women still face a measurable risk of developing cysts, even years after their last menstrual period. Understanding your risk factors and symptoms is key to early detection and proper management.
After menopause, the hormonal environment changes dramatically. Even though the ovaries slow down, they still produce small amounts of hormones that can influence cyst development.
Common causes and risk factors include:
Women with a personal or family history of ovarian or breast cancer may also face higher risks. Regular checkups with an ovarian cysts specialist can help detect changes early and prevent complications.
The symptoms of ovarian cysts after menopause can be subtle at first. Some women may not feel any discomfort until the cyst grows larger or presses on nearby organs.
Common symptoms include:
If a cyst ruptures or causes ovarian torsion (twisting of the ovary), the pain can be sudden and severe. This situation requires immediate medical attention.
Diagnosis begins with a pelvic exam, during which a healthcare provider feels for any abnormalities. If a cyst is suspected, imaging tests help confirm the size, shape, and characteristics of the mass.
The most common imaging techniques include:
If the cyst appears complex or solid, further testing may be necessary. A CA-125 blood test measures a protein often elevated in ovarian cancer. After menopause, high CA-125 levels may indicate the need for closer evaluation.
Doctors also review your medical history to identify risk factors such as BRCA gene mutations, prior cancers, or family history of ovarian or breast cancer. These details guide the next steps in diagnosis and treatment.
Although ovarian cysts are more common before menopause, several types can still occur afterward. Each type has different causes, risks, and treatment considerations.
Functional cysts: These are linked to the menstrual cycle and usually disappear after menopause. However, remnants can occasionally persist.
Cystadenomas: These develop from the cells on the ovary’s surface. They can grow quite large but are often benign.
Dermoid cysts: Also known as teratomas, these form from embryonic cells and may contain tissue such as hair or fat. They are typically noncancerous but can cause discomfort if they enlarge.
Endometriomas: Women with a history of endometriosis may still develop these cysts after menopause, especially if small amounts of endometrial tissue remain active.
Malignant cysts: Although less common, the risk of ovarian cancer increases after menopause. Any complex or solid cyst must be carefully assessed by a gynecologic specialist.
Treatment depends on the cyst’s type, size, and symptoms. Not all cysts require surgery; some can be safely monitored.
Watchful waiting: If the cyst is small, appears benign, and CA-125 levels are normal, doctors may recommend observation with follow-up ultrasounds.
Medication and hormone management: Pain relievers may help reduce discomfort. In some cases, hormone therapy may help stabilize hormone levels and prevent further cyst formation.
Surgical treatment: If the cyst is large, painful, or appears suspicious, removal may be necessary.
Laparoscopic surgery is often the preferred method when the cyst is small and appears benign. This minimally invasive approach allows for faster recovery and less discomfort.
If you experience persistent pelvic pain, bloating, or changes in bleeding patterns, it is best to seek medical attention promptly. Do not ignore sudden, sharp pain, fever, or vomiting, as these could signal a ruptured cyst or ovarian torsion.
Postmenopausal women should schedule routine pelvic exams and follow their provider’s recommendations for imaging or blood testing. Regular evaluations help detect changes early, offering the best outcomes for long-term health.
If symptoms occur alongside hormonal changes or other menopause-related issues, consulting a menopause specialist can help address overlapping concerns more effectively.
Being diagnosed with an ovarian cyst after menopause can feel stressful, but most cysts are benign and manageable. Maintaining open communication with your doctor and attending follow-up appointments helps track any changes.
Staying active, managing weight, and eating a balanced diet may also support overall hormonal and metabolic health. Women with a history of ovarian cysts should avoid delaying medical evaluation for new pelvic symptoms.
Here at The Women’s Center, we understand how unsettling pelvic discomfort can feel, especially after menopause. Our experienced specialists offer advanced diagnostic imaging, personalized treatment plans, and compassionate guidance for every stage of your health.
We help you feel confident, informed, and supported throughout your care.



Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read More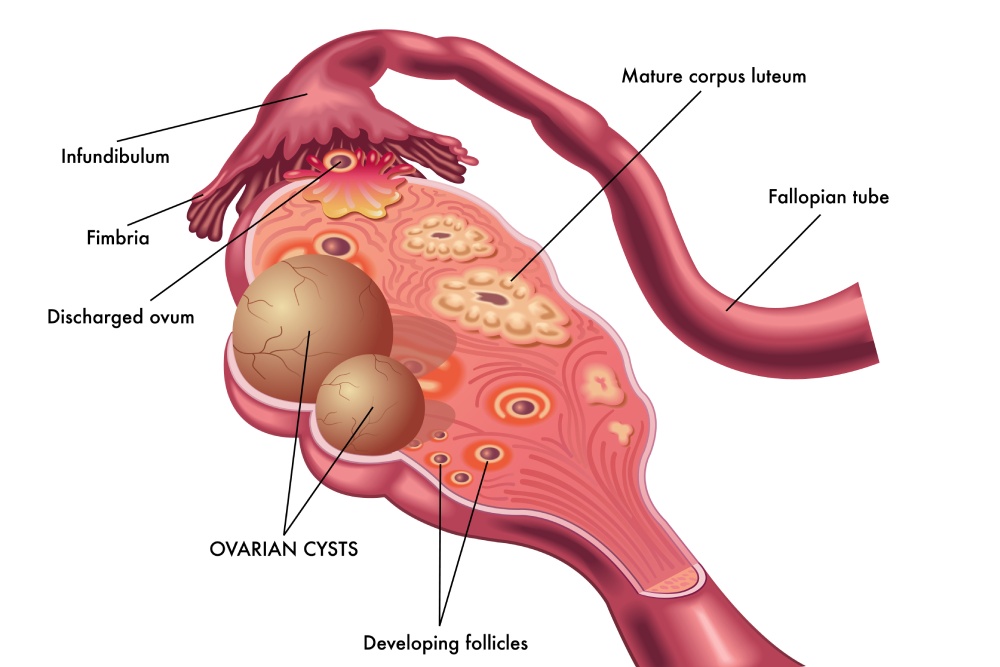
Ovarian cysts after menopause may seem uncommon, but they can still develop even when the...
Read More
Uterine fibroids are one of the most common benign growths affecting women. By age 50,...
Read More