
Surgical Solutions: Exploring Hysterectomy As A PCOS Treatment
Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read MoreDeciphering the differences between a 2D and a 3D mammogram is crucial for informed health decisions. The traditional 2D mammogram takes x-rays of breast tissue in flat images, while the advanced 3D version, also known as tomosynthesis, captures multiple slices of breast tissue, providing a more detailed picture. This distinction enhances the detection of breast abnormalities, potentially leading to earlier intervention.
At The Women's Center, we offer sophisticated 3D mammogram services, matching high standards of care with the nuanced needs of women's health. Our state-of-the-art technology peels back layers of breast tissue digitally, giving our experts a clear view to better distinguish harmless structures from concerning areas, effectively reducing the need for follow-up imaging.

Traditional 2D mammograms generate flat images of the breast, providing a two-dimensional view that has been the standard in breast cancer screening for decades. While effective for many women, the limitation of 2D mammography lies in its inability to offer depth perception. This shortcoming can sometimes result in overlapping tissues in the images, which can obscure or mimic cancerous growths, potentially leading to repeated screenings or unnecessary biopsies.
On the other hand, 3D mammography constructs a layered, three-dimensional image of the breast. This innovative approach allows radiologists to examine breast tissue layer by layer, significantly reducing the confusion caused by tissue overlap seen in 2D images. The depth perception provided by 3D images grants physicians a clearer view, enhancing the likelihood of detecting abnormalities with greater accuracy and confidence. This advancement in technology marks a significant step forward in personalized preventive care, offering women a more detailed, and potentially less stressful, screening experience.
Women with dense breast tissue stand to benefit markedly from 3D mammography. Dense breast tissue, characterized by less fat and more connective and glandular tissue, appears white on mammograms – the same color as potential malignancies, making it challenging to discern between normal and abnormal areas with 2D imaging. The effectiveness of 3D mammography in these scenarios becomes evident as its enhanced imaging capability allows for a more precise separation of dense tissue from potential concerns, thereby facilitating early detection of breast cancer, which is critical for successful treatment and outcomes.
The significance of this technology is particularly profound for women who have been historically underserved by traditional mammography due to their dense breast tissue. The expanded accessibility of 3D mammograms across Central Florida represents a proactive approach to inclusive healthcare, ensuring that all women, regardless of their breast tissue composition, have access to reliable and accurate breast cancer screening options.
Despite the advantages of 3D mammography in terms of detection accuracy, it’s essential to consider the factors where 2D mammograms may still hold value. Principally, 2D mammograms are quicker and more cost-effective than their 3D counterparts. This speed and economic efficiency make 2D mammograms accessible to a wider range of the population, providing an essential service within holistic healthcare frameworks, particularly in environments where access to advanced technology might be limited by financial or infrastructural constraints.
Nonetheless, the decision between a 2D and 3D mammogram should not solely rest on cost and convenience. Given the superior detail and increased detection capabilities of 3D mammography, women, especially those with dense breast tissue or at a higher risk of breast cancer, may find the benefits far outweigh the higher cost and slightly longer procedure time. Engaging in conversations with healthcare providers about the advantages of each method allows women to consider their personal health history, risks, and preferences in the context of these advancements in breast screening technologies.
While the benefits of 3D mammograms in terms of detection and accuracy are clear, women should be informed that these tests do expose them to slightly higher levels of radiation compared to 2D mammograms. This increase is due to the additional images that 3D mammography requires to create a multi-layered view of the breast. Nonetheless, the amount of radiation is still within the safe limits approved by the FDA. The priority remains on safeguarding patient health, and thus, the slightly higher exposure is carefully measured to ensure it does not outweigh the benefits derived from the enhanced diagnostic capabilities of 3D mammograms.
The consideration of radiation exposure is a delicate balance between risk and reward. It is a testament to the advancements in medical technology that these screenings remain within safety standards while offering superior imaging capabilities. Women should have comprehensive dialogues with their healthcare providers about the risks associated with radiation and the frequency of mammograms they should undergo, taking into consideration their overall risk factors, age, and family history.
Access expert mammography screenings Orlando residents trust. Our commitment at The Women's Center, with nine convenient locations, extends to offering precise and personalized mammography. By using both 2D and 3D imaging as needed, we tailor breast screening to each woman's unique circumstances, ensuring a comprehensive and compassionate approach to preventative care.

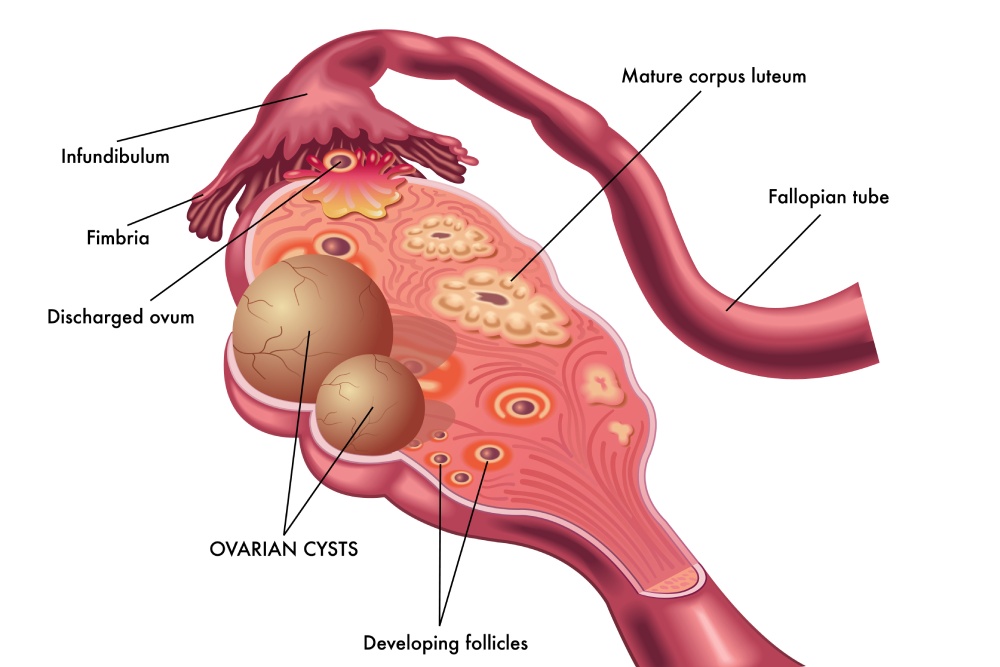


Polycystic Ovary Syndrome affects millions of women worldwide, often bringing challenges like irregular periods, hormonal...
Read More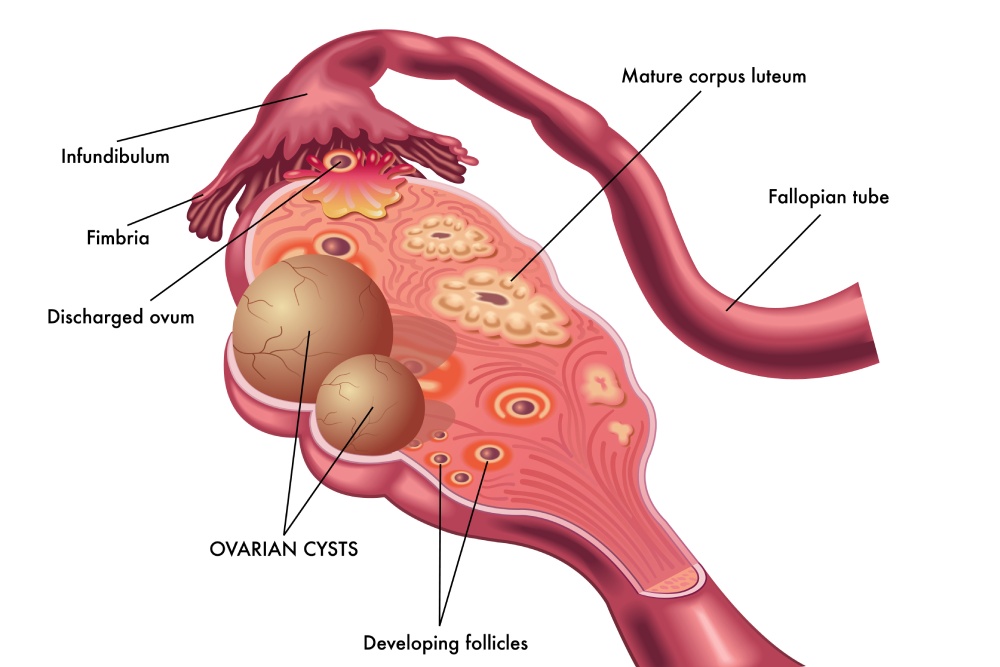
Ovarian cysts after menopause may seem uncommon, but they can still develop even when the...
Read More
Uterine fibroids are one of the most common benign growths affecting women. By age 50,...
Read More